Storm Warning: The Telltale Signs of Mini Strokes

Before a tornado hits, it typically announces itself with some classic indicators: huge hail, a dark, almost green sky, and emergency sirens. By listening to these warnings from Mother Nature, we have more time to take cover before seeing a twister.
When something is wrong with our health, bodies will often provide indicators. Ignoring symptoms of a serious illness is like going out on the porch to watch a funnel cloud roar into the yard while a harried meteorologist, pleading with us to take cover, plays on TV in the background.
Take strokes, for example.
The Warning of Mini Strokes
Prior to a stroke, the body may receive a warning in the form of a transient ischemic attack (TIA), commonly referred to as “mini stroke.” Professionals in neurology are moving away from using the term “mini stroke” because the word “mini” makes it sound a lot less serious than it is.
While TIAs are usually temporary and do not cause permanent brain damage, The Big One may be on the way. After a TIA, 10% will have a major stroke in two days, 15% will have a stroke in three months, and 25% will have a recurrent event within three months, which is another TIA or a major stroke.
A major stroke, which can cause permanent injury or death, is as dangerous as an F5 twister headed in your direction.
After a TIA:
Risk Factors for Transient Ischemic Attack
There is an increased risk for a TIA as a result of poorly controlled risk factors such as:
- High blood pressure
- High cholesterol
- Diabetes
- Heart condition
- Smoking
What Happens During a TIA
During a TIA, there is a temporary disruption in the blood supply to a part of the brain. This is usually caused by a temporary blood clot in a blood vessel of the brain.
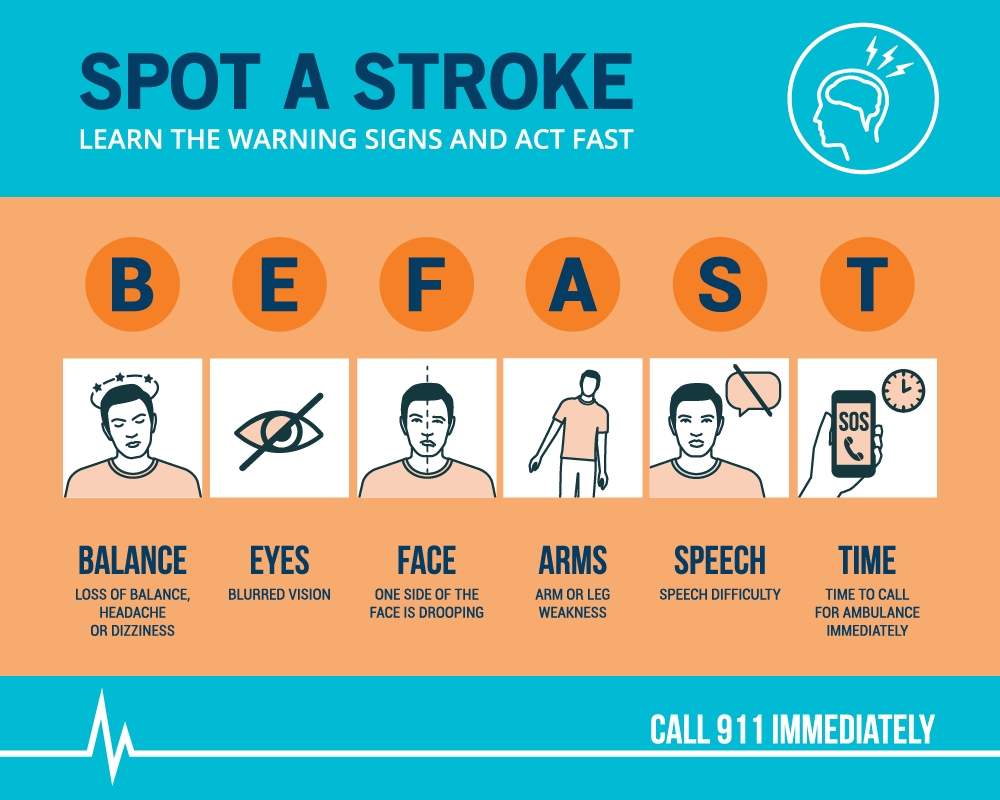
Symptoms of TIAs
The symptoms of a TIA are similar to those of a regular stroke but are usually milder and not as long-lasting. They can include sudden:
- Weakness or numbness in the face, arm, or leg, typically on one side of the body
- Confusion or trouble speaking or understanding speech
- Trouble seeing in one or both eyes
- Trouble walking, dizziness, loss of balance, or coordination
- Severe headache with no known cause
TIA symptoms typically last for a few minutes to a few hours and resolve on their own. If symptoms persist or worsen, it could indicate a major stroke.
Medical Care for TIAs
Call 911
A TIA is a medical emergency. The symptoms experienced during a TIA may go away quickly, but they may return. It is not okay to drive. By calling 911, EMS can perform an evaluation and provide safe transportation to the emergency room.
Testing & Preventive Medication
When the patient gets to the hospital, their doctor will likely perform a physical exam, blood tests, and brain scans to find where their TIA originated. Depending on the cause of their TIA, their treatment may include medications to lower blood pressure, prevent future blood clots, lower cholesterol, surgery to remove blockages in the blood vessels, and more.
Recovery and Prevention of Future Strokes
Self-Care
Stroke survivors must take care of themselves after a TIA to reduce their risk of stroke in the future. It’s always easier said than done, but after a TIA, stroke survivors should eat a balanced diet, exercise, quit smoking, get adequate sleep, and take their medication. Prioritizing oneself can be difficult, but self-care is paramount during this time.
Emotional Support
Stroke survivors should also prioritize their mental health. They may find it difficult to cope with or process what happened. Some ways to improve their emotional well-being include:
- Practicing mindfulness or meditation
- Spending time with loved ones
- Physical therapy
- Joining a support group (click the link for the support group schedule)
- Talking to a therapist or counselor
Emotional Changes After TIA or Stroke
Nearly one-quarter of people who have TIAs or strokes also experience emotional changes. This could be a result of the brain injury or an emotional response to having a stroke. Four common emotional changes are quick, impulsive style, apathy, pseudobulbar affect (PBA), and depression.
Quick, Impulsive Style
Many stroke survivors want to do things that they can’t do. This includes driving or walking without a needed aid. A stroke survivor’s facial expressions may lessen, making their feelings less obvious to the people around them.
Apathy
Some survivors may not appear to care about anything. Apathy may be mistaken for depression. The best treatment for apathy is to get the person active and moving. Give them choices and help them to choose to do something.
Pseudobulbar Affect (PBA)
This is also known as emotional lability or reflex crying. Stroke survivors cry more easily and may laugh uncontrollably with sudden mood changes. This is a physical effect of the stroke. The lability often lessens over time. Many times, the family needs to treat these mood changes like hiccups and continue with conversations. Don’t tell the person not to cry.
Depression
Half of all stroke survivors experience depression. Depression results from the biochemical changes that occur in the brain due to the stroke. Depression can make stroke recovery far more difficult. Signs of depression include persistent sadness, anxious or negative mood, loss of interest in hobbies, feeling of worthlessness, fatigue, insomnia, irritability, weight changes, and suicide threats.
Change the Forecast
By heeding the warning of a TIA, patients may be able to change the forecast of their health.
If you have had a TIA or are a stroke survivor, you can receive a customized treatment plan from a board-certified Singing River neurologist. Have your primary care provider send a referral to Singing River Neurology to get started.
Don’t have a primary care provider? Learn more about establishing yourself as a patient.