Peripheral Artery Disease
There are an estimated 7 to 12 million people in the United States who suffer from Peripheral Artery Disease, or PAD, leading to approximately 150,000 leg amputations per year. If you have foot sores, leg pain, tingling, and heavy or cold legs and feet, you may PAD. Learn more about the disease, how to get diagnosed, and the many treatment options available that can help you improve your vascular health and avoid limb loss.
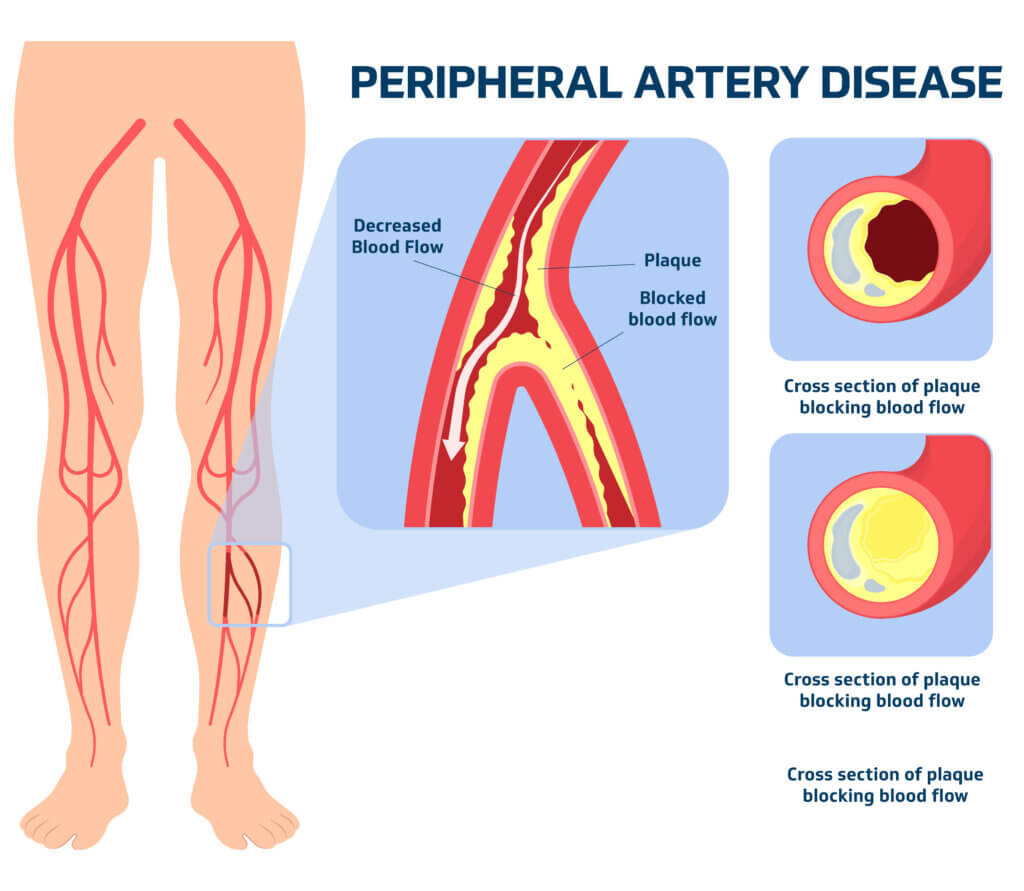
What is Peripheral Artery Disease (PAD)?
Peripheral Artery Disease, or PAD, is a condition in which the blood vessels outside your heart—most often in the legs—become narrowed due to plaque buildup (atherosclerosis).
This buildup is made of a sticky substance of fat, cholesterol, and other materials, and it restricts blood flow to your legs, leading to discomfort, particularly during physical activities like walking.
Anyone can develop PAD, but certain factors increase your risk:
- Age: People over 50 are more likely to develop PAD.
- Lifestyle factors: Smoking, poor diet, and lack of physical activity raise the risk.
- Medical conditions: High blood pressure, diabetes, and high cholesterol are key contributors.
What are the symptoms of PAD?
PAD often develops slowly, and in its early stages, it may cause no symptoms. Here are common signs to watch for:
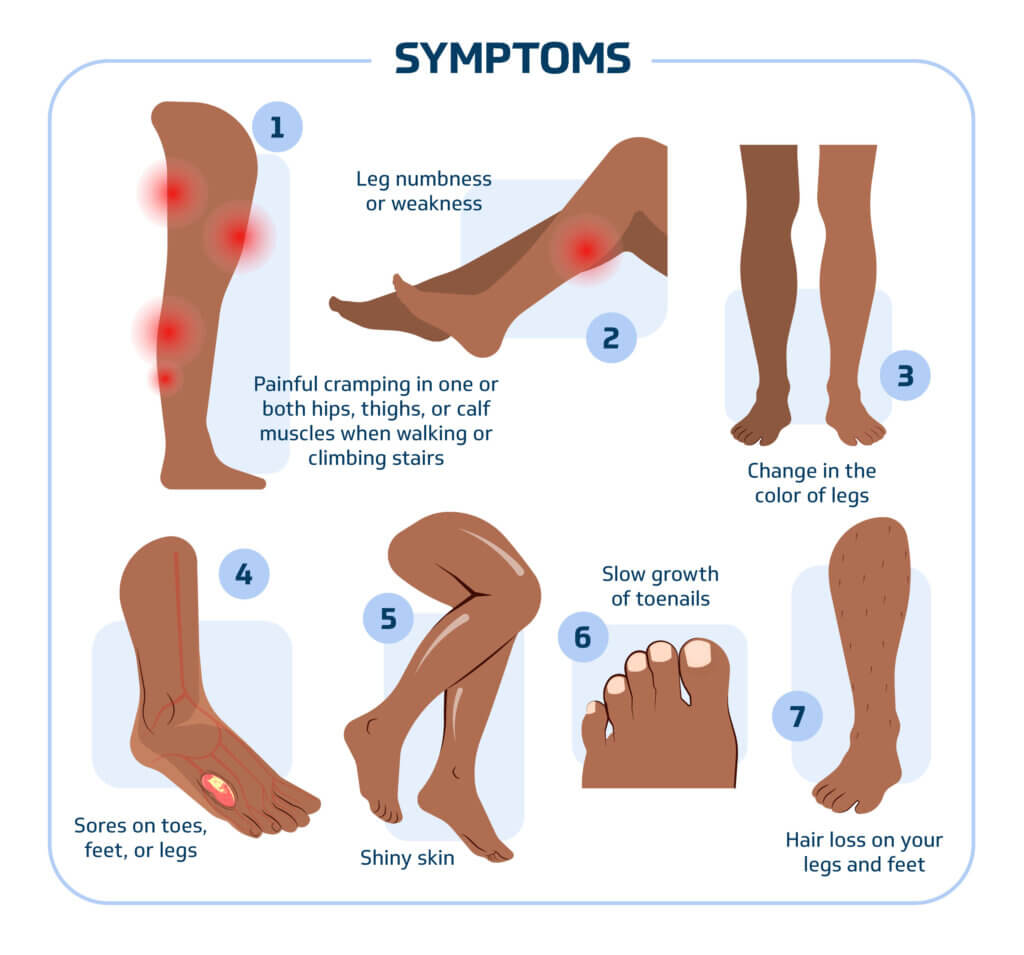
- Leg pain or cramping when walking or climbing stairs (claudication), which eases with rest
- Numbness or weakness in the legs
- Color or temperature change in lower leg or foot, especially when compared to the other leg
- Sores on your toes, feet, or legs that heal slowly or don’t heal at all
- Shiny skin on the legs
- Slow growth of toenails
- Hair loss on the feet and legs
How is PAD diagnosed?
Diagnosing PAD involves a few simple tests, often performed by a doctor specializing in vascular conditions, such as the interventional cardiologists at Singing River Cardiology.
- Physical Exam: A doctor may check for weak pulses in the legs.
- Ankle-Brachial Index (ABI): This is a quick, painless test comparing the blood pressure in your ankle with the blood pressure in your arm. A lower pressure in the leg can indicate PAD.
- Imaging Tests: Ultrasounds, CT scans, or MRIs may be used to visualize blood flow and detect narrowed or blocked arteries.
How is PAD related to diabetes and diabetic neuropathy?
Diabetes is a significant risk factor for PAD. Over time, high blood sugar levels can damage blood vessels, leading to plaque buildup and reduced circulation. In addition, diabetic neuropathy—nerve damage caused by prolonged high blood sugar—can mask the pain that typically signals PAD, such as leg pain while walking. This can delay diagnosis and treatment, increasing the risk of severe complications.
Patients with diabetes should be especially vigilant for PAD symptoms, even if they do not feel pain, and should have regular checkups with their healthcare provider to monitor circulation and nerve health.
How is PAD treated?
Treatment for PAD often involves lifestyle changes, medications, and sometimes procedures or surgery.
Lifestyle Changes
- Smoking cessation
- Diabetes management
- Healthy diet
- Regular exercise
Medications
- Blood thinners: help prevent blood clots from forming
- Statins: lower cholesterol
- Blood pressure medication: lower your blood pressure
Procedures
For more severe cases of PAD, doctors may recommend:
Angioplasty (Percutaneous Coronary Intervention)
Angioplasty is a minimally invasive procedure that uses a catheter to insert a small balloon into a narrowed or blocked artery. The doctor inflates the balloon in order to widen the artery, improving blood flow.
Stents
Often performed with an angioplasty, stenting involves placing a small mesh tube (stent) in the artery after it has been widened by the balloon. The stent helps keep the artery open and maintains improved blood flow.
Atherectomy
When plaque is too hard or calcified for angioplasty and stenting alone to be effective, a cardiologist may perform an atherectomy. During this procedure, a catheter with a tiny cutting instrument is used to manually remove plaque buildup from the inside of an artery to improve blood flow.
Bypass Surgery
This is a more invasive surgical procedure that takes place when angioplasty is not feasible. During bypass surgery, the surgeon creates a new route for blood to flow by grafting a healthy blood vessel taken from another part of the body (usually the leg, arm, or chest) to bypass the blocked section of the artery.
What are the complications of PAD?
Without treatment, PAD can lead to complications, including:
- Critical Limb Ischemia (CLI): This is a severe reduction in blood flow, which can cause sores, infections, and even tissue death (gangrene) in extreme cases. After one year, at least 25% of patients with CLI undergo at least one major limb amputation.
- Increased Risk of Heart Attack and Stroke: Because PAD often accompanies widespread atherosclerosis, it can increase the risk of heart attacks and strokes.
When should I see a doctor?
If you experience pain in your legs while walking that eases with rest or notice any of the other PAD symptoms, it’s important to see a healthcare provider. Early diagnosis can help prevent more severe complications and improve your quality of life.
Singing River’s Interventional Cardiologist Dr. Scott Laura and Vascular Surgeon Dr. Gregory McGee are trained in treating heart-related blockages and experts at treating peripheral vascular conditions like PAD.
Their goal is to help patients with PAD restore blood flow and improve their symptoms, avoiding more invasive surgeries such as amputations.
Make an appointment by having your provider to refer you to Singing River Cardiology or Singing River Cardiovascular Surgery. Then, call the location of your preference to make an appointment.
Don’t have a provider? Learn how to establish a primary care provider at Singing River.




